Who Can Benefit from DBT for OCD?
Dialectical Behavior Therapy (DBT) can be highly beneficial for individuals struggling with Obsessive-Compulsive Disorder (OCD). People who struggle with intense emotional responses to their obsessions and compulsions often find DBT useful. Dr. Katie Flanigan-Landeros utilizes DBT to help patients develop mindfulness, distress tolerance, and emotional regulation skills, allowing them to better manage OCD symptoms and improve their mental well-being. For more information, contact us or schedule an appointment online. We are conveniently located at 400 Continental Blvd FL 6, Suite A El Segundo, CA 90245.
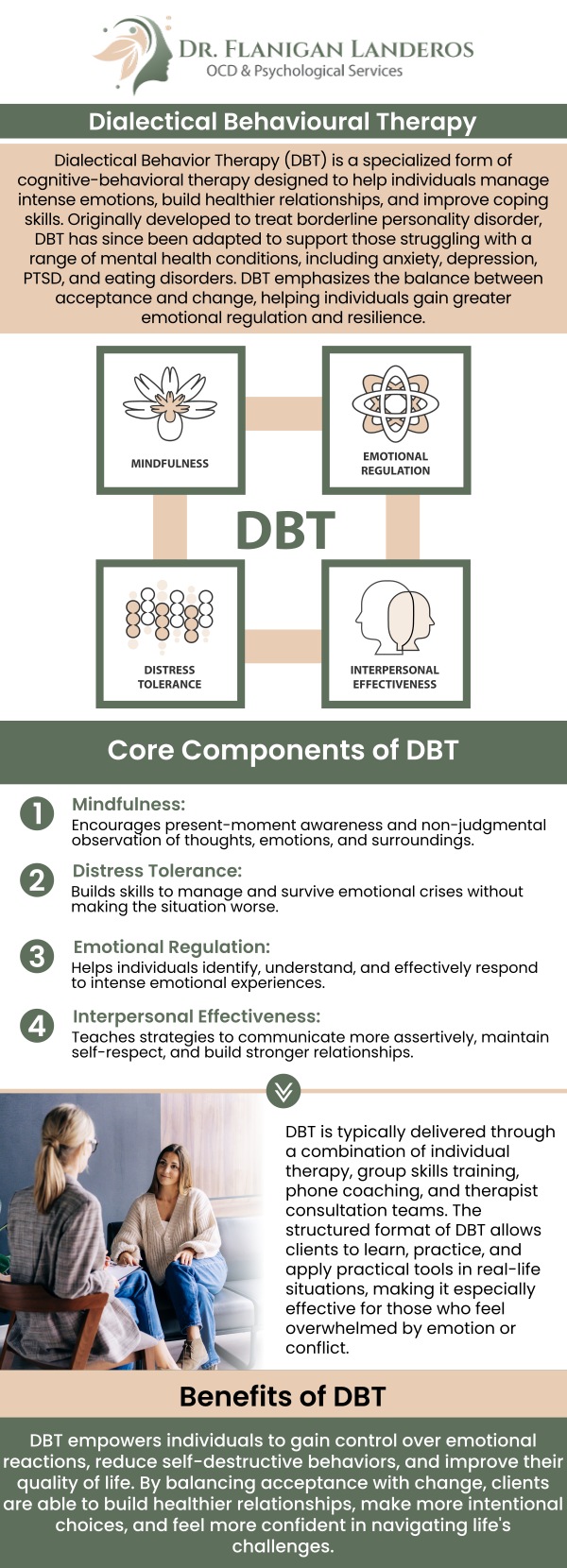
Table of Contents:
Can DBT help people with OCD who also have difficulty managing emotions?
Who should consider DBT as a treatment for OCD?
Can DBT be helpful for people with severe or chronic OCD?
Who would not benefit from DBT for OCD?
How Dr. Katie Flanigan Landeros Helps Manage OCD with DBT Techniques
Dr. Katie Flanigan Landeros understands that living with obsessive-compulsive disorder (OCD) can be incredibly challenging—especially when intense emotions like anxiety, shame, or frustration make it difficult to participate fully in treatment. While exposure and response prevention (ERP) is the gold-standard approach for OCD, some clients find that their emotional reactions can get in the way of making progress.
This is where dialectical behavior therapy (DBT) can be a valuable addition to your care. Originally designed for individuals struggling with borderline personality disorder and chronic suicidality, DBT has been adapted to help people with a wide range of mental health conditions, including those with OCD who also experience emotional dysregulation.
Dr. Flanigan Landeros incorporates DBT skills training as part of a comprehensive OCD treatment plan for clients who need extra support managing their emotions.
DBT focuses on four main skill areas:
• Mindfulness: Helping you become more aware of obsessive thoughts and urges without automatically reacting to them.
• Distress Tolerance: Equipping you with techniques to manage the intense discomfort or anxiety that can arise during exposure exercises or when resisting compulsions.
• Emotion Regulation: Teaching you strategies to identify, understand, and manage mood swings or overwhelming feelings that may accompany OCD.
• Interpersonal Effectiveness: Enhancing your relationships and communication skills which can reduce stress and emotional triggers that may worsen OCD symptoms.
For individuals with OCD who also struggle with depression, anxiety, or self-harming behaviors, integrating DBT with ERP can make treatment more effective and manageable. Dr. Flanigan Landeros draws on her experience with both OCD and DBT to create a personalized treatment plan that addresses your unique needs. If you or a loved one is interested in learning how DBT can support OCD recovery, Dr. Katie Flanigan Landeros is here to help. Together, we can build the tools and strategies needed to manage distress, regulate emotions, and achieve lasting improvement in your quality of life.
At Dr. Katie Flanigan Landeros OCD & Psychological Services, we recognize that obsessive-compulsive disorder (OCD) can present in complex and unique ways, especially when accompanied by intense emotions or co-occurring mental health challenges. DBT (dialectical behavior therapy) is not typically the first-line treatment for OCD, but there are specific circumstances where it may be a beneficial adjunct or alternative.
Here are some individuals who might consider DBT as part of their treatment plan for OCD:
Co-occurring Emotional Dysregulation or Personality Disorders:
• Individuals with OCD who also struggle with intense emotional dysregulation, mood swings, or self-destructive behaviors (e.g., self-harm or suicidal tendencies) may benefit from DBT’s focus on emotion regulation and distress tolerance skills. DBT is particularly effective for people with conditions like borderline personality disorder, which often co-occurs with OCD in some cases.
History of Trauma or PTSD:
• Those with OCD who also have a history of trauma or post-traumatic stress disorder (PTSD) may find DBT helpful. DBT’s focus on mindfulness, self-soothing, and emotional regulation can provide tools to manage trauma-related emotional responses, which might be exacerbated by OCD.
Severe OCD with Difficulty Tolerating Distress:
• For individuals with severe or chronic OCD who struggle to tolerate distressing emotions and may engage in avoidance or compulsions to cope with anxiety, DBT can offer strategies for managing overwhelming emotions without resorting to compulsive behaviors.
Interpersonal and Relationship Difficulties:
• People with OCD who experience significant relationship or interpersonal issues may find DBT useful due to its focus on improving interpersonal effectiveness. DBT teaches skills for navigating relationships and communicating more effectively, which can be challenging for those whose OCD symptoms interfere with daily functioning.
OCD Not Fully Addressed by Traditional Therapies:
• Some individuals whose OCD symptoms are not sufficiently managed by traditional treatments like ERP (exposure and response prevention) or CBT (cognitive behavioral therapy) might consider DBT as an additional or supplementary treatment. DBT can help address the emotional and interpersonal difficulties that sometimes accompany OCD, especially when traditional therapies do not fully meet all the individual’s needs.
When OCD Triggers Intense Emotional Responses:
• For those whose OCD triggers extreme emotional responses—such as anger, frustration, or hopelessness—DBT’s focus on mindfulness and distress tolerance can help individuals respond to these emotional challenges in a healthier way, reducing the impact of negative emotions on their OCD.
In most cases, DBT would not replace traditional treatments like ERP for OCD, but could serve as an additional tool for managing associated emotional difficulties or co-occurring mental health conditions. Dr. Katie Flanigan Landeros is experienced in assessing when DBT or DBT-informed interventions may be indicated, ensuring you receive personalized care that addresses the full spectrum of your needs.
At Dr. Katie Flanigan Landeros OCD & Psychological Services, we understand that obsessive-compulsive disorder (OCD) can be complex and deeply challenging—especially when accompanied by difficulties with emotional regulation or co-occurring conditions such as anxiety, depression, or impulsivity.
Dialectical behavior therapy (DBT) can be helpful for some individuals with severe or chronic OCD, but it is not typically the first-line treatment for the disorder. DBT is primarily designed to help individuals with emotional dysregulation, self-destructive behaviors, and conditions like borderline personality disorder. While DBT includes components like mindfulness, distress tolerance, and emotion regulation, which may offer support to those with OCD, it does not specifically target the core symptoms of OCD, such as intrusive obsessions and compulsive behaviors.
That said, for individuals with severe or chronic OCD who also struggle with intense emotional dysregulation, trauma history, or interpersonal difficulties, DBT might provide valuable supplementary skills. The emotional regulation techniques taught in DBT can help manage the distress that often accompanies OCD, particularly in cases where OCD symptoms contribute to significant emotional upheaval or difficulties in relationships. However, for OCD specifically, the gold-standard treatment remains exposure and response prevention (ERP) therapy, which directly targets the compulsions and obsessions through exposure and response prevention exercises.
In some cases, a combination of DBT and ERP may be used, but ERP would generally be the primary therapeutic approach for treating OCD symptoms. If you or a loved one is struggling with severe or chronic OCD and finds that emotional regulation is a significant challenge, Dr. Katie Flanigan Landeros is here to help. She offers compassionate, evidence-based care that draws on both ERP and DBT principles to support long-term recovery and improved quality of life.
At Dr. Katie Flanigan Landeros OCD & Psychological Services, we are committed to providing evidence-based care for individuals struggling with obsessive-compulsive disorder (OCD) and related conditions. One therapy that is often asked about is dialectical behavior therapy (DBT). Dialectical behavior therapy (DBT) is a highly effective treatment for individuals struggling with emotion regulation, self-destructive behaviors, and borderline personality disorder, but it may not be the most suitable for those primarily dealing with obsessive-compulsive disorder (OCD). While DBT includes components of mindfulness and emotional regulation that can benefit some individuals with OCD, it is not specifically designed to target the core symptoms of OCD, such as intrusive thoughts and compulsive behaviors.
Individuals who may not benefit from DBT for OCD include those who require more targeted, evidence-based treatments like exposure and response prevention (ERP) therapy, which is the gold standard for OCD treatment. DBT’s emphasis on emotional regulation and interpersonal effectiveness might not directly address the need for systematic exposure to feared stimuli and the prevention of compulsive rituals, which is at the heart of ERP therapy.
Additionally, DBT may not be effective for individuals with OCD who have not yet developed the skills or readiness to engage in DBT’s more complex strategies, particularly those dealing with more severe forms of OCD. For those individuals, a more focused treatment like ERP or cognitive-behavioral therapy (CBT) would likely be a more effective approach for addressing their symptoms. While DBT is an excellent resource for certain mental health concerns, our primary recommendation for those with OCD is to pursue targeted, proven therapies such as ERP. Dr. Flanigan Landeros is dedicated to offering specialized, evidence-based care for OCD and can help you determine the most effective treatment plan for your unique needs.
Dr. Katie Flanigan Landeros utilizes dialectical behavior therapy (DBT) techniques to help individuals manage obsessive-compulsive disorder (OCD). DBT, originally developed to treat borderline personality disorder, has proven effective in treating OCD, especially when there are co-occurring emotional regulation difficulties or high distress tolerance issues. Dr. Landeros incorporates DBT skills such as mindfulness, emotional regulation, distress tolerance, and interpersonal effectiveness to support patients in managing the anxiety and frustration that often accompany OCD.
By integrating DBT with traditional OCD treatments like cognitive behavioral therapy (CBT) and exposure and response prevention (ERP), Dr. Landeros provides a comprehensive, well-rounded approach to treatment. This combination helps individuals develop healthier coping strategies, tolerate distressing thoughts without resorting to compulsive behaviors, and improve their overall quality of life. Dr. Landeros tailors her use of DBT techniques to each patient’s unique needs, ensuring personalized care that addresses both the symptoms of OCD and the emotional challenges that may arise.
For more information, contact us or schedule an appointment online. We are conveniently located at 400 Continental Blvd FL 6, Suite A El Segundo, CA 90245. We serve patients from El Segundo CA, Santa Monica CA, Inglewood CA, Gardena CA, Torrance CA, Hawthorne CA, Culver City CA, Westmont CA, West Los Angeles CA and surrounding areas.

Check Out Our 5 Star Reviews


Additional Services You May Need
▸ Anxiety
▸ Depression
▸ OCD
▸ Relationships
▸ Individual Psychotherapy
▸ Psychological Testing
▸ ADHD
▸ Telehealth
▸ Seasonal Mood Changes
▸ Cognitive Behavioral Therapy
▸ Life Transition
▸ Acceptance and Commitment Therapy (ACT)
▸ Exposure With Response Prevention (ERP)
▸ Dialectical Behavior Therapy (DBT)
▸ OCD Subtypes
▸ Perfectionism
▸ Group Therapy

Additional Services You May Need
▸ Anxiety
▸ Depression
▸ OCD
▸ Relationships
▸ Individual Psychotherapy
▸ Psychological Testing
▸ ADHD
▸ Telehealth
▸ Seasonal Mood Changes
▸ Cognitive Behavioral Therapy
▸ Life Transition
▸ Acceptance and Commitment Therapy (ACT)
▸ Exposure With Response Prevention (ERP)
▸ Dialectical Behavior Therapy (DBT)
▸ OCD Subtypes
▸ Perfectionism
▸ Group Therapy